Who really controls the privacy of medical records—and what do changing laws mean for you? This article explores the debate between protecting sensitive health information and ensuring efficient access for care, unpacking current events and the most misunderstood HIPAA rules you need to know. Let’s look at where safety, empowerment, and digital innovation collide.
Key Takeaways
- The privacy of medical records is under constant pressure from changing regulations, new technology, and evolving patient expectations.
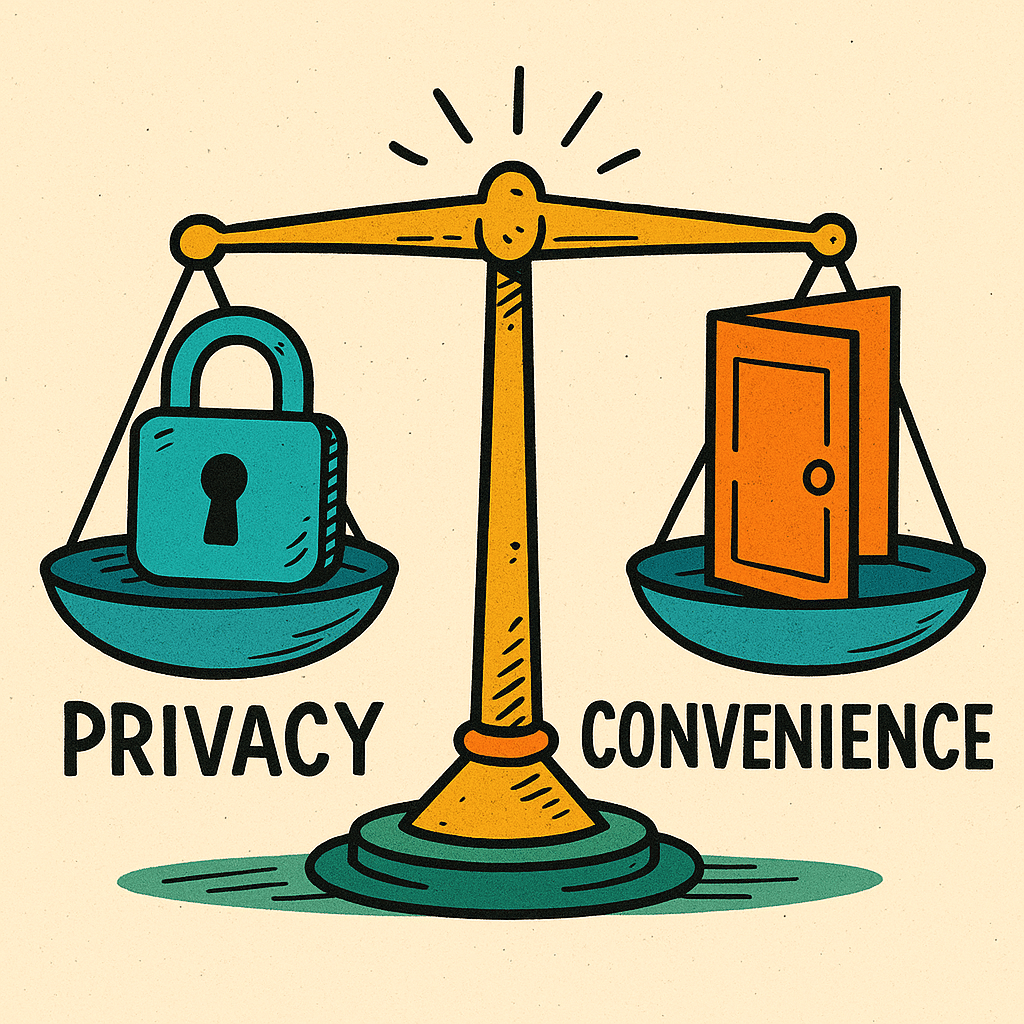
- Overly strict privacy protections can hinder care, while too much access increases the risk of data breaches—finding the right balance is essential.
- Recent rulings and laws, including updates to HIPAA and new state mandates, are reshaping how health data is shared and protected.
- Patients, providers, and organizations must stay informed about common HIPAA misconceptions to safeguard confidentiality and empower care.
Privacy of Medical Records: The Ongoing Debate
The privacy of medical records is not just a technical concern—it’s deeply personal. Every time a patient enters an exam room, they trust that their most intimate health details will remain between themselves and their care team. Many people believe that their health information should be strictly protected at all costs, with no exceptions. That trust forms part of the bedrock of our healthcare system. Why? Because breaches of privacy can have far-reaching consequences far beyond a single embarrassing disclosure. From identity theft to social stigma, unauthorized access to medical records has the potential to disrupt lives, careers, and even personal relationships.
It’s easy to argue that privacy should always take priority. “Medical information is among the most sensitive data anyone possesses,” says Dr. Tracy Fischer, a New York-based psychiatrist. “If patients fear their records may be shared without consent, they may hesitate to disclose details that are crucial for treatment.” Many privacy advocates point out that legislation like the Health Insurance Portability and Accountability Act (HIPAA) was designed to give patients peace of mind—a guarantee that healthcare providers will safeguard their records, subject to strict penalties for violations.
Beyond personal concerns, there are broader implications for the privacy of medical records. Governments and regulatory bodies set boundaries to prevent misuse of genetic information, reproductive health history, mental health diagnoses, or other records that could be weaponized by employers, insurers, or even law enforcement. Recent headlines remind us how quickly things can change: “A federal judge in Texas vacated the new HIPAA rule designed to strengthen privacy protections for reproductive health information,” reports the HIPAA Journal. This kind of legal uncertainty can deeply unsettle patients, who may not always keep up with shifting protections.
For some, the fear surrounding digital records can feel almost existential. When every aspect of your health history is digitized, encrypted, and scattered across dozens of electronic health record systems, it’s reasonable to worry about who might access it. Privacy-conscious patients favor granular control: the ability to decide who sees what, and when, especially in situations involving mental health or a newly diagnosed condition. The right to keep some aspects of your medical story confidential is a matter of dignity, not just policy.
Yet insisting on rigorous privacy protections comes with a cost. Medical providers face enormous administrative complexity to comply with privacy mandates, and sometimes, that very effort can create friction or even disruption in care delivery. There is a risk that overly cautious policies make essential information inaccessible when it’s needed most, inadvertently putting patients at risk.

Access to Medical Records: The Case for Convenience and Safety
There’s another side to this story—the argument for greater access to medical records. Today’s healthcare is collaborative, fast-paced, and often distributed across multiple organizations. The privacy of medical records remains paramount, but providers and patients also benefit from the ease of secure sharing. Instant access to complete health histories saves time, reduces repeated tests, and can even save lives in emergencies.
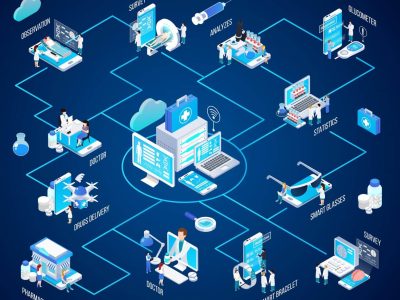
Many clinicians argue that the greatest danger comes not from over-sharing, but from too little sharing. Dr. Bruce Bassi notes, “I frequently see patients who have had to repeat evaluations simply because prior records weren’t accessible in time.” In practice, delayed record-sharing leads to redundant procedures and frustrated patients—hardly a recipe for high-quality medicine. Healthcare is increasingly reliant on interoperability, with EHR platforms like Epic and Cerner exchanging data using standardized methods (e.g., FHIR, HL7). The privacy of medical records is safeguarded, but well-designed systems make it possible for authorized professionals to quickly access and act on critical health information.
From the patient’s perspective, access means empowerment. You can download your labs, share your vaccination status, or send your allergy list to a new provider on demand. Laws like HIPAA enshrine your right to access your own medical records, no matter your ability to pay. This isn’t just a convenience—it’s a necessity for modern care coordination. Seamless access allows for second opinions, telehealth visits, and prompt interventions in a crisis.
Access also means justice and transparency. Patients with chronic conditions, rare diseases, or reproductive health needs should be able to control, carry, and review their own data without barriers. Overly restrictive privacy protocols may unintentionally harm these groups by complicating the transfer of essential information from specialist to specialist or from state to state. Increasingly, healthcare organizations must find a way to embrace both security and usability—so everyone benefits.
Despite these advantages, greater access brings its own challenges. The more data is shared, the greater the risk of breaches, accidental disclosures, or unauthorized use. Both personal error and systematic vulnerabilities can threaten the privacy of medical records. Stricter identity verification, encryption, and audit trails may help, but nothing guarantees perfect protection. Striking a balance is harder than it looks.
Nuances and Trade-offs: Where Privacy Meets Access
Real life is full of gray areas. Patients want privacy and access—often both in the very same moment. For instance, someone may want their cancer diagnosis shared with an oncology team, but not with their employer. They might consent to sharing substance use history for treatment, but insist on keeping mental health records private. Modern health record platforms attempt to solve this with granular permissions, time-limited sharing, and transparent audit logs.
Healthcare providers are caught in the crossfire. On one hand, regulations demand strict compliance, with significant fines for violations. On the other, patient care depends on rapid, accurate information exchange. Overcautious interpretation of privacy rules is one of the most misunderstood concepts of HIPAA. According to the HIPAA Guide, “Many providers believe that HIPAA prohibits all forms of information sharing, but the law explicitly allows PHI disclosure for treatment, payment, and healthcare operations.”
Patients, too, are often misinformed. Some think “HIPAA-certified” means a system is officially blessed by the government, while others fear that minor disclosures for care coordination constitute a privacy breach. In fact, the law provides broad rights for patients to access their own records, even if bills are unpaid, and allows limited sharing for public health or law enforcement under clearly defined circumstances.
Nuanced privacy of medical records shouldn’t be a barrier to innovation. Emerging solutions include “privacy by design” architecture, patient-driven consent forms, and real-time tracking of record access. Artificial intelligence, wearable health tech, and telemedicine are all raising new questions: how do we balance convenience, precision, and confidentiality? The answer is rarely simple, but the best platforms communicate risks and options transparently.

Current Events Shaping the Privacy of Medical Records
Recent rulings, law changes, and regulatory proposals continue to shape this landscape. The overturned HIPAA reproductive health rule in Texas has left some women rightly concerned about the fate of sensitive reproductive data. Meanwhile, the national update to the HIPAA Security Rule will require providers nationwide to adopt multi-factor authentication, real-time risk assessments, and stronger encryption—changes that will both protect and complicate access for clinicians and patients alike. Texas’s new law mandating U.S.-only localization for health records underscores how state laws are becoming just as important as federal mandates in defining the privacy of medical records. What applies in one state may not apply in another, with direct consequences for patients seeking care across borders.
As one data security analyst put it, “Regulation isn’t just a federal story anymore; states may now set privacy standards that go beyond HIPAA, or in some cases, roll back protections.” The stakes are high, not just for the privacy of medical records, but for the integrity of the entire health system. Both patients and organizations must stay nimble, informed, and proactive—sometimes going beyond the law to protect what matters most.

Common Misunderstandings About HIPAA
HIPAA only applies to covered healthcare entities, not all organizations handling health info (e.g., schools, fitness apps).
Providers can share information for treatment without getting consent every time.
“HIPAA-certified” is a marketing term—there’s no such true government approval.
Patients retain the right to access their records regardless of outstanding bills.
The law does not block sharing between providers for legitimate medical care; misinterpretation can hinder safety and quality.
Conclusion
The debate over privacy of medical records is not merely academic—it affects how we live, heal, and trust our healthcare system. Personal privacy and broad access are both essential, but too much of one may dilute the benefits of the other. Recent events have shown that laws and standards are dynamic, shaped by courts, states, and technology itself. Staying informed—about policies, myths, and options—is one of the best protections both patients and providers can have. The privacy of medical records will remain a central issue in medicine, demanding solutions that respect dignity, support care, and meet the demands of a changing world.
“Who can legally access my medical records under HIPAA?”
Under HIPAA, your medical records can be legally accessed by healthcare providers directly involved in your treatment, payment processing, or essential healthcare operations—without needing your specific written permission every time. However, employers, life insurers, schools, or mobile health apps are generally not covered by HIPAA and cannot access your medical records unless you explicitly authorize them. Law enforcement and public health authorities may also obtain access under strictly regulated circumstances, but only when necessary and allowed by law. You yourself always retain the right to access your own records, even if you have unpaid medical bills.
Summary
This article explores the complex debate over the privacy of medical records, weighing the need for strict confidentiality against the benefits of easier access for care. It argues both sides, highlights key nuances, and incorporates recent legal changes—including new HIPAA updates and state laws—shaping how health data is protected and shared. Clear explanations of common HIPAA misconceptions help patients and providers understand their rights and responsibilities in today’s shifting digital healthcare landscape.
If you need help or want to learn more, you can contact us directly. We’re here to support you every step of the way.
Related Topics
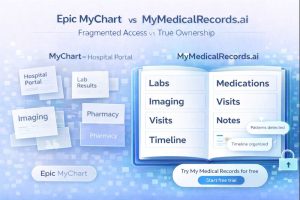
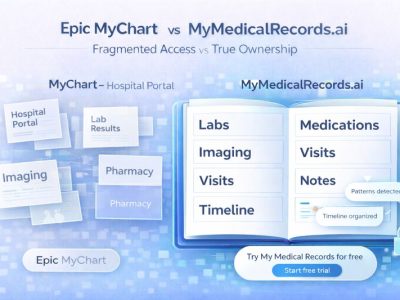
Epic MyChart vs. MyMedicalRecords.ai: Portal Access vs. True Ownership
Epic MyChart vs. MyMedicalRecords.ai: Portal Access vs. True Ownership Meta description: Epic MyChart only shows records from one hospital system. MyMedicalRecords.ai aggregates 100% of your
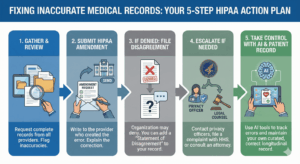
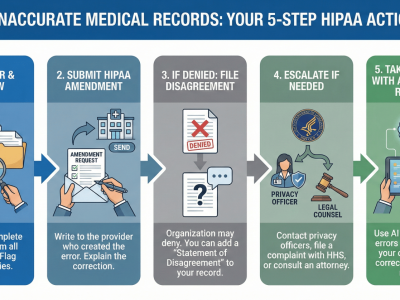
What to Do If There Is Inaccurate Data in Your Medical Record
The chart that does not match you You probably discovered the inaccurate medical records error because something routine went wrong: a prior authorization denied, a
From Chaos to Clarity: A Family Caregiver’s Guide to Unified Health Records
Here’s what nobody tells you about caregiving: The hardest part isn’t watching your loved one struggle with their diagnosis. It’s trying to keep track of
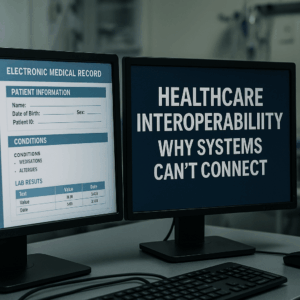
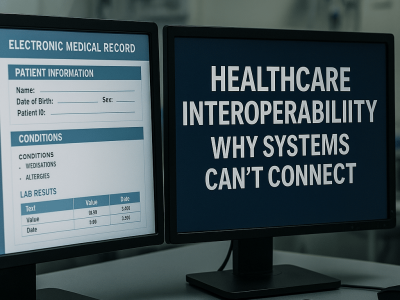
Healthcare Interoperability: Why Systems Can’t Connect
Healthcare interoperability is the ability of different healthcare systems, devices, and applications to seamlessly share, understand, and use patient data across organizations and geographic boundaries.

How to Merge Medical Records from Multiple Doctors and Avoid Errors & Duplicates
Learn how to merge medical records from multiple doctors, avoid duplicate entries, and reduce errors. Use AI tools like My Medical Records to simplify the process.
What Happens to Your Medical Records After a Doctor Retires or a Clinic Closes?
Learn how to merge medical records from multiple doctors, avoid duplicate entries, and reduce errors. Use AI tools like My Medical Records to simplify the process.