Healthcare interoperability is the ability of different healthcare systems, devices, and applications to seamlessly share, understand, and use patient data across organizations and geographic boundaries. This digital connectivity enables healthcare providers to access complete patient information instantly, improving care quality while reducing costs and medical errors. Modern interoperability relies on standards like FHIR (Fast Healthcare Interoperability Resources) and HL7 to ensure secure, real-time data exchange between hospitals, clinics, labs, and patient health apps.
Key Takeaways
Healthcare interoperability enables systems, devices, and applications to exchange and use patient data seamlessly, improving continuity of care.
Barriers are multifaceted—including outdated technology, business incentives, and complex privacy regulations—not just technical shortcomings.
Patients are directly affected by repeated tests, delays in care, and the burden of managing their own records.
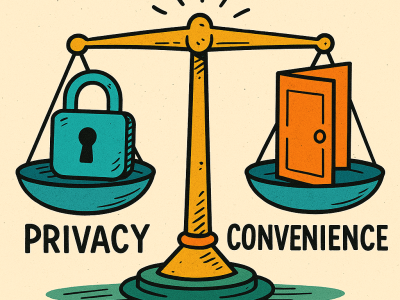
Strict privacy safeguards protect sensitive data but may unintentionally limit information sharing between clinicians.
Slow adoption has pros and cons—it ensures careful implementation and compliance but prolongs inefficiencies and costs.
Table of Contents
What is Healthcare Interoperability and Why It Matters
Healthcare interoperability sounds complicated, but the concept is simple: it’s making sure your medical information can follow you wherever you go for care. Think of it like your smartphone—you can text someone whether they have an iPhone or Android because the systems can “talk” to each other. Healthcare interoperability aims to do the same thing with your medical records.
This capability is far more than a convenience; it’s a cornerstone of modern, high-quality care. When systems can seamlessly share data, a doctor in the emergency room can instantly access your medication list and known allergies, preventing a dangerous drug interaction. Your new specialist can review a complete medical history from your family doctor, saving you from repeating lengthy explanations and tests. It also empowers you as a patient, allowing you to access and share your own health data with any provider.
Without this digital connectivity, care often becomes fragmented. Patients are left to be their own record-keepers, carrying paperwork between appointments and filling out the same forms multiple times. This not only causes frustration and delays but also introduces risks if crucial details are forgotten. Ultimately, interoperability ensures that all members of your care team have the full picture, leading to more accurate diagnoses, better treatment plans, and improved safety.
Why Medical Records Can't Talk to Each Other
The inability of medical records to communicate isn’t just a technical problem—it’s a complex mix of business, regulatory, and technological challenges.
The Three Main Barriers
Outdated Technology: Many healthcare organizations run decades-old systems that weren’t designed for data sharing. Different systems use different formats—like one measuring in inches and another in centimeters. Upgrading is expensive and risky, like renovating a house while people live in it.
Business Competition: EHR companies often make it difficult to share data with competitors, and healthcare organizations sometimes view patient data as a competitive advantage. Implementation costs for interoperability can seem prohibitive for cash-strapped organizations.
Legal Complexity: HIPAA and privacy laws create legitimate concerns about data sharing violations and massive fines. When information is shared between organizations, liability questions arise—who’s responsible if shared data causes medical errors? Different states also have varying requirements for record retention and patient consent.

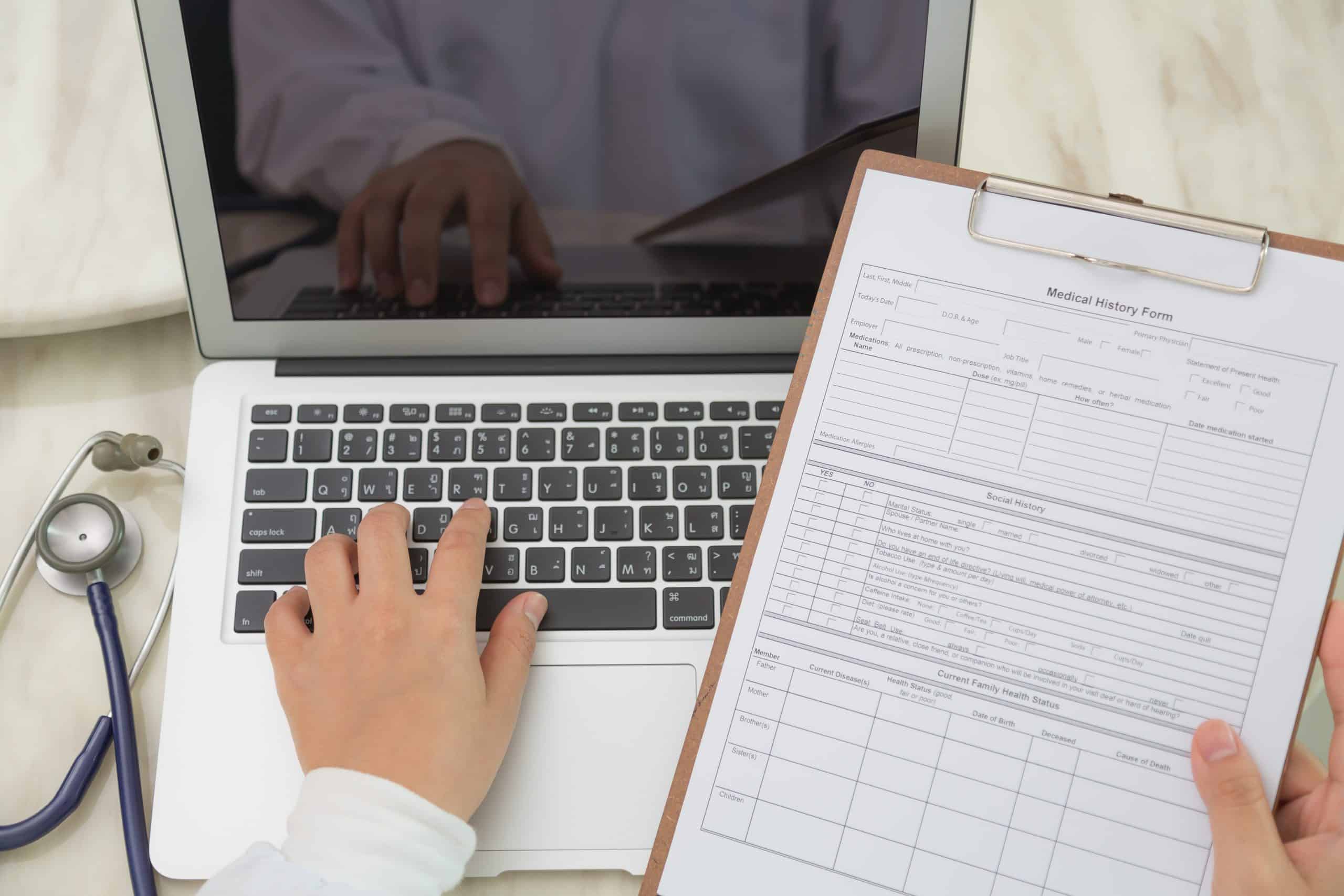
Patients Experience: Paperwork, Delays, and Tests
For patients, a lack of interoperability shows up as repeated paperwork, delayed appointments, and duplicate tests. When records don’t transfer smoothly between clinics or hospitals, patients are often left to coordinate their own care, remembering medication lists and past diagnoses or physically carrying documents to new providers.
“I frequently see patients who have had to repeat evaluations simply because prior records weren’t accessible in time,”says Dr. Bruce Bassi, MD, MS, Medical Director and Founder of TelepsychHealth. “It’s frustrating for patients, but providers are equally concerned about making decisions without full information.”
In this context, the lack of interoperability in healthcare systems has a profound and negative impact on patient care. The inability of different healthcare systems to communicate and share data seamlessly leads to a fragmented patient experience. Patients often find themselves as the de facto couriers of their own medical history, a task that is both burdensome and prone to error. They must recall intricate details about their past health, including specific drug dosages, surgical dates, and past test results. This puts them in a precarious position, as any missed detail could affect the quality of their care.
This issue not only frustrates patients but also poses a significant risk to their safety. Dr. Bassi’s observation about repeated evaluations is a common scenario, highlighting the inefficiency and potential for medical error. When providers like him lack a complete and timely picture of a patient’s health history, they’re forced to make decisions with incomplete information. This can lead to unnecessary costs from redundant tests and, more critically, could result in a misdiagnosis or an inappropriate treatment plan. The problem extends beyond mere inconvenience, evolving into a critical issue of patient safety and quality of care.
The Hidden Costs and Risks
Redundant testing and administrative inefficiencies contribute to higher overall costs in the healthcare system. At the same time, immediate, systemwide data sharing raises legitimate privacy and security concerns. Patients and providers alike worry about unauthorized access or misuse of sensitive medical data.
“Healthcare organizations have to balance two responsibilities: providing accurate, coordinated care and protecting patient confidentiality,” Dr. Bassi notes. “These goals sometimes feel at odds, even though both are essential.”
These competing priorities create a significant challenge for modern healthcare. The push for seamless data sharing, while promising to reduce redundant testing and streamline care, must navigate the complex landscape of patient data privacy. Each time a patient’s information is digitally transferred, there’s a potential risk of a data breach. This is a critical concern, especially as cyber threats become more sophisticated.
Patients need to feel confident that their most personal health information is secure. Similarly, providers and healthcare organizations face strict regulations, like HIPAA in the United States, that mandate the protection of this data. A single security lapse can lead to severe financial penalties and a loss of public trust.
Therefore, the development of interoperable systems must be coupled with robust security measures and clear policies that ensure data is only accessed by authorized personnel for legitimate medical purposes. The core issue is not simply the sharing of data, but the safe and secure sharing of it, which requires a careful balance of technological innovation and stringent privacy protocols.

Why Organizations Move Slowly
Even with modern standards like FHIR and HL7, interoperability is not simply a technical upgrade. Many hospitals rely on older electronic health record (EHR) platforms that are costly and disruptive to replace. Some organizations are reluctant to invest in new infrastructure without clear financial incentives. Others worry about liability if incorrect or incomplete data is shared.
Pros of slow adoption: Careful implementation minimizes errors, avoids major workflow disruptions, and ensures regulatory compliance.
Cons of slow adoption: Patients face delays, providers lack timely information, and costs from inefficiency continue to mount.
Business and Regulatory Pressures
Healthcare data is valuable—not just clinically but economically. Some EHR vendors and health systems are cautious about open sharing, concerned about losing competitive advantage. At the same time, privacy laws such as HIPAA are designed to protect patients but can feel restrictive to organizations uncertain about how to comply.
Pros of strict controls: Patient information stays protected, reducing the risk of breaches and misuse.
Cons of strict controls: Overly cautious policies may prevent necessary information from reaching the clinicians who need it.
Moving Toward Practical Solutions
Progress will likely involve a combination of better technology, clearer legal guidance, and cultural change in how organizations view data sharing. Patients are increasingly able to access and carry their own health information, which may encourage systems to align with these expectations.
“Patients want care that’s coordinated no matter where they go,” Dr. Bassi says. “The challenge is to achieve that without compromising accuracy, security, or trust.”
What Happens to Your Medical Records?
When a doctor retires or a clinic shuts down, your medical records don’t just vanish. Medical records are legally protected even if your doctor retires or a clinic closes.
Summary:
Healthcare interoperability aims to ensure that patient information follows individuals wherever they seek care, improving safety, efficiency, and treatment outcomes. Despite advances in data standards such as HL7 and FHIR, adoption is slowed by legacy systems, regulatory complexity, and differing business incentives. While cautious implementation protects privacy and minimizes risk, it also creates inefficiencies that frustrate patients and providers alike. Achieving meaningful interoperability will require balancing security with accessibility, fostering collaboration among stakeholders, and building systems that serve both clinical needs and patient expectations.
If you need help or want to learn more, you can contact us directly. We’re here to support you every step of the way.
Related Topics:
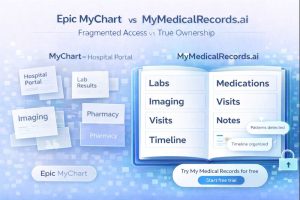
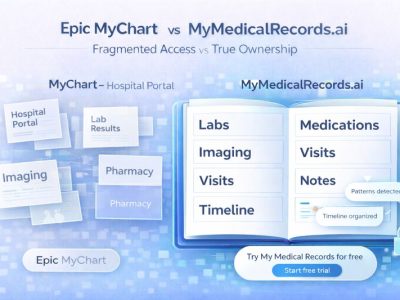
Epic MyChart vs. MyMedicalRecords.ai: Portal Access vs. True Ownership
Epic MyChart vs. MyMedicalRecords.ai: Portal Access vs. True Ownership Meta description: Epic MyChart only shows records from one hospital system. MyMedicalRecords.ai aggregates 100% of your
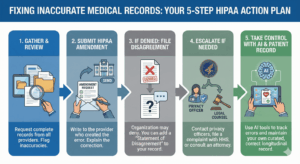
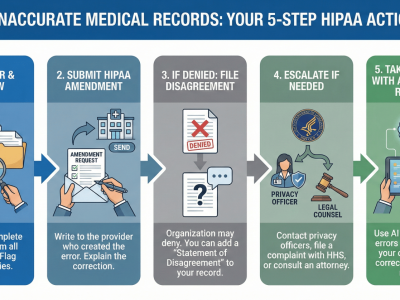
What to Do If There Is Inaccurate Data in Your Medical Record
The chart that does not match you You probably discovered the inaccurate medical records error because something routine went wrong: a prior authorization denied, a
From Chaos to Clarity: A Family Caregiver’s Guide to Unified Health Records
Here’s what nobody tells you about caregiving: The hardest part isn’t watching your loved one struggle with their diagnosis. It’s trying to keep track of
Privacy vs Access: Finding the Right Balance in Your Digital Health Record
Healthcare interoperability is the ability of different healthcare systems, devices, and applications to seamlessly share, understand, and use patient data across organizations and geographic boundaries.

How to Merge Medical Records from Multiple Doctors and Avoid Errors & Duplicates
Learn how to merge medical records from multiple doctors, avoid duplicate entries, and reduce errors. Use AI tools like My Medical Records to simplify the process.
What Happens to Your Medical Records After a Doctor Retires or a Clinic Closes?
Learn how to merge medical records from multiple doctors, avoid duplicate entries, and reduce errors. Use AI tools like My Medical Records to simplify the process.